Ami Kothari
In recent years, telemedicine has emerged as a game-changer in the healthcare industry, offering patients and providers a new way to interact with each other. This was especially evident during the Covid-19 pandemic when the usage of telemedicine services spiked.
In particular, telemedicine has made a significant impact on the field of mental and behavioural healthcare. Mental health conditions such as anxiety, depression, and substance abuse are prevalent worldwide, yet access to care can be challenging due to stigma, cost, and limited resources. Telemedicine online platform development has provided a means of addressing these barriers and improving access to care for needy patients.
In this article, we will explore how telemedicine is bridging the gap in mental and behavioural healthcare and the benefits it offers to both patients and providers.
5 Major Challenges in Traditional Mental and Behavioural Healthcare
Challenges in traditional mental and behavioural healthcare can be numerous and complex. These range from social issues to technical and accessibility issues. Here are some of the major challenges that traditional mental and behavioural healthcare faces:
Limited access
One of the biggest challenges in traditional mental and behavioural healthcare is limited access to care. People living in rural or remote areas may not have access to mental healthcare services or may have to travel long distances to receive care. This can be particularly difficult for those who have mobility or transportation issues.
Stigma
Another major challenge in traditional mental and behavioural healthcare is mental illness stigma. Many people feel ashamed or embarrassed to seek help for their mental health issues or may fear being judged by others. This can prevent them from seeking the care they need.
High costs
Traditional mental and behavioural healthcare can also be costly, particularly for those without insurance or limited financial resources. This can create a significant barrier to accessing care for those who need it.
Provider shortages
There is a shortage of mental health providers in many areas, making it difficult for individuals to receive timely and effective treatment. This is particularly true in rural areas, where the number of mental health providers is often lower than in urban areas.
Time constraints
Traditional mental and behavioural healthcare also faces time constraints, particularly in scheduling appointments and providing follow-up care. This can make it difficult for individuals to receive the ongoing care they need to manage their mental health issues.
Bridging the Gap Between Telemedicine in Mental and Behavioral Healthcare: 4 Steps
Mental health is crucial to overall well-being, yet it is often neglected or stigmatized. The World Health Organization reports that one in four people globally will be affected by mental or neurological disorders at some point. Unfortunately, mental health care is still not easily accessible to all individuals due to various factors such as social stigma, lack of healthcare professionals, and limited access to healthcare facilities, particularly in rural areas.
However, telemedicine has brought about significant improvements in the mental healthcare system. Telemedicine for mental health has become a vital tool in bridging the gap between patients and healthcare providers. It has revolutionised mental healthcare delivery by providing a way to reach and treat patients who otherwise would not have access to care.
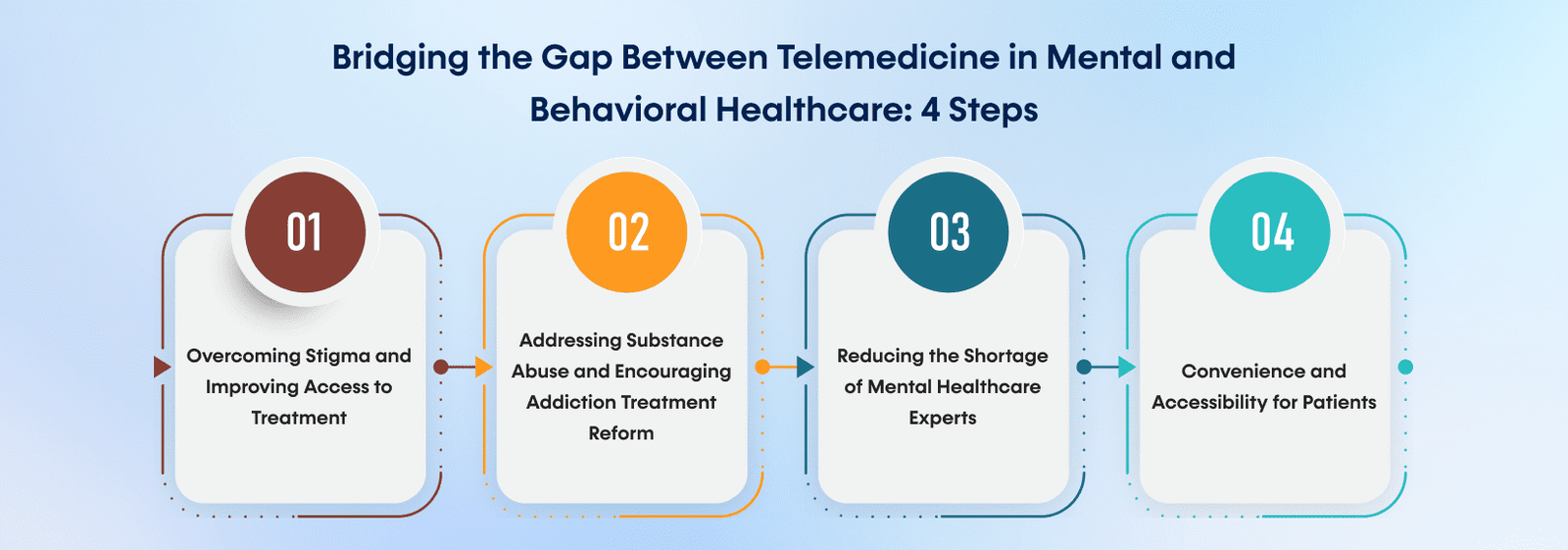
Here are some changes that remote access telemedicine software can bring to providing mental health treatment.
1. Overcoming Stigma and Improving Access to Treatment
Telemedicine for mental health has the potential to break down the stigma surrounding mental illnesses and make it easier for people to access proper treatment. By providing care remotely, patients can receive treatment from the comfort and privacy of their homes without worrying about being seen going to a mental health clinic.
2. Addressing Substance Abuse and Encouraging Addiction Treatment Reform
Telemedicine for mental health is also effective in addressing the opioid epidemic and the substance abuse that it entails, thus encouraging reform in addiction treatment. Telepsychiatry allows for easier access to medication-assisted treatment, which has been shown to be effective in treating opioid addiction. It also enables patients to access care more frequently, improving outcomes.
3. Reducing the Shortage of Mental Healthcare Experts
Telepsychiatry can help alleviate the shortage of mental healthcare experts. It allows healthcare providers to reach patients in remote or underserved areas, increasing access to care for those who may not have otherwise been able to receive it. This can also help reduce appointment wait times and improve overall patient outcomes.
4. Convenience and Accessibility for Patients
Finally, telemedicine for mental health is more convenient and easily accessible for people struggling with mental illnesses. It eliminates the need for patients to travel to a physical clinic, which can be difficult for those with limited mobility or transportation options. This can make it easier for patients to stick to their treatment plans and receive the care they need on a regular basis.
Challenges and Future of Telemedicine in Mental and Behavioural Healthcare
Despite the numerous benefits of telemedicine in mental and behavioural healthcare, it also faces several challenges that hinder its effectiveness. One major challenge is the difficulty in assessing nonverbal cues and body language through video consultations. The inability to perform physical exams or tests remotely also gets in the way, as some conditions require one-on-one physical tests.
Another challenge is the digital divide. Some patients may not have access to the internet or a smartphone, which makes it impossible for them to use telemedicine services. Moreover, some patients may not be comfortable with technology, which can make it challenging for them to receive treatment through telemedicine. There is also the issue of privacy and security. Though there are some challenges in implementing Telemental Health, we can overcome them by using the latest healthcare technologies. Mental health professionals have to ensure that the patient’s data is secure and that there is no breach of confidentiality during the telemedicine session.
What is the Future Hold for Telemedicine in Mental and behavioural health?
The future of telemedicine in mental and behavioural healthcare looks promising. With the increasing demand for mental health services, telemedicine provides a viable solution for reaching more patients and providing timely treatment. Telemedicine also allows mental health professionals to monitor patient’s progress and adjust their treatment plans accordingly.
Technology advancements are also improving telemedicine’s effectiveness in mental and behavioural healthcare. For example, virtual reality therapy is becoming more prevalent in treating anxiety and phobias. Moreover, artificial intelligence is being used to detect early signs of mental illness and provide personalised treatment plans. Here is how you can implement Telehealth & Telemedicine in your hospital & clinic.
Summing Up
Telemedicine has revolutionised the delivery of mental and behavioural healthcare, making it more accessible. This has broken down the stigma surrounding mental illnesses and made it easier for people to access proper treatment. Telemedicine has also allowed easier access to medication-assisted treatment and reduced the shortage of mental healthcare experts. Challenges in traditional mental and behavioural healthcare include limited access, stigma, high costs, provider shortages, and time constraints. However, the future of telemedicine in mental and behavioural healthcare is bright, with potential for further development and expansion.
To benefit from telemedicine apps and websites for your mental and behavioural healthcare needs, contact us at EMed HealthTech, a leading telemedicine app development company. We provide customised telemedicine app development services that suit your particular needs. Our client-centric approach ensures all your needs are met through the custom healthcare app we create. Mark your presence in the mental healthcare industry with a sturdy telemedicine app to cover your technical needs.
Related posts

Telemedicine
Telemedicine in 2025: Top Mobile App Development Trends Shaping the Future of Healthcare
As we move into 2025, telemedicine is emerging as a key player in healthcare innovation. The rapid evolution of telemedicine app development redefines patient care and makes healthcare more accessible, flexible, and efficient.
Read more
Telemedicine
The Future of Telemedicine: Trends to Watch in 2025
Telemedicine has rapidly become one of the most revolutionary aspects of modern healthcare. With its role in medical services expanding each year, the future of telemedicine is filled with incredible potential.
Read more
Telemedicine
Basic Features of a Successful Telemedicine Platform
Telemedicine has grown to be a crucial component of contemporary healthcare, providing a more convenient and effective means of communication between patients and medical professionals.
Read more









